Scoliosis on X-Ray: Severity and Treatment Options
Scoliosis isn’t merely a curious condition of the spine-it is a real challenge affecting millions. Insights drawn from recent research shed light on its prevalence, severity, and treatment approaches. For instance, approximately 2–3% of the population, or about seven million people in North America, face this condition according to recent research. These numbers remind us that clarifying the meaning of an X-ray result is vital for both patients and clinicians as they make important treatment decisions.
The goal of this discussion is to explore how modern diagnostic techniques, particularly the interpretation of X-ray findings, enhance the understanding of scoliosis severity and shape treatment options. Among the recent developments in the field is an innovative X-ray classification system that redefines how radiographic features are communicated. This article delves into what that means for patients, families, and healthcare providers, offering a deep dive into classifications, severity assessments, and treatment techniques that continue to evolve as research advances.
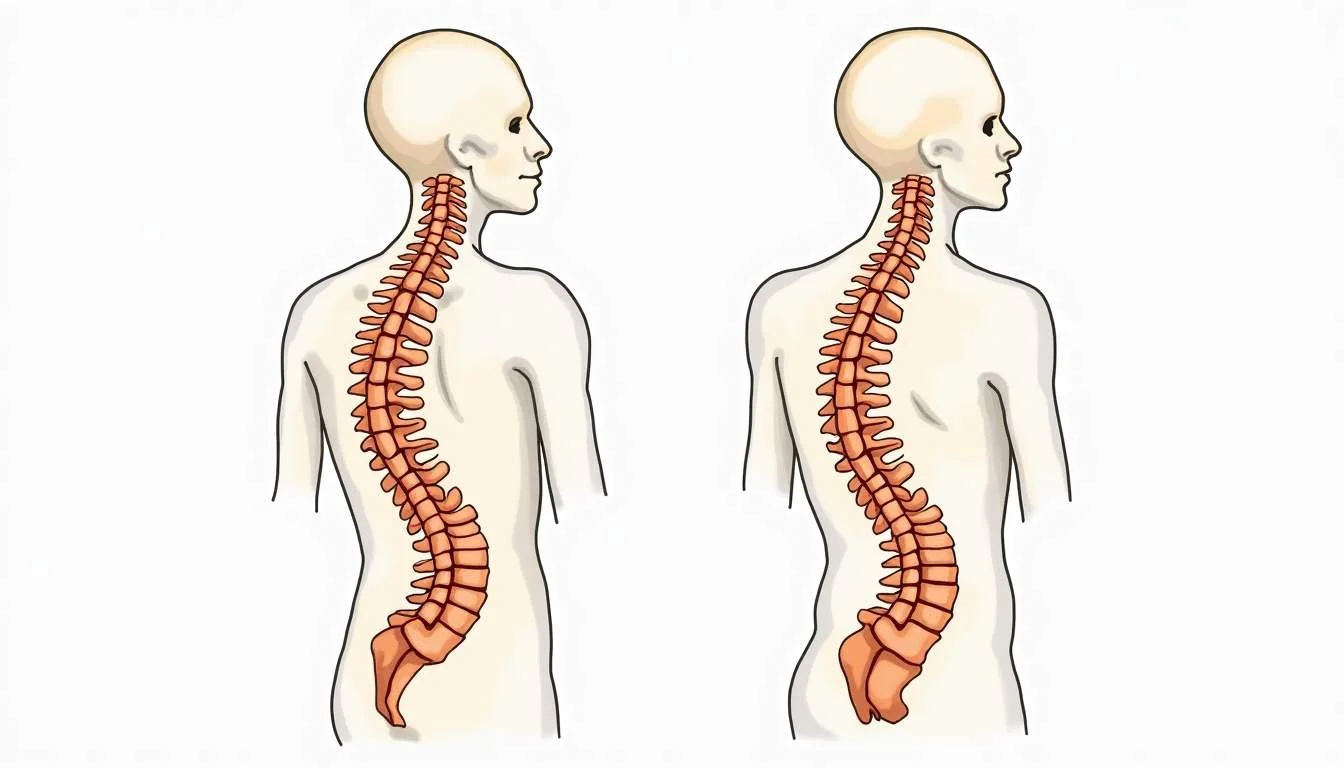
What is Scoliosis?
Scoliosis is a condition characterized by an abnormal curvature of the spine. The curvature can develop during childhood or adolescence, though it also appears later in life. In many cases, the condition presents itself in a mild form and does not progress to cause significant complications; however, in others, scoliosis can lead to discomfort and restricted movement, sometimes necessitating early intervention.
Recent research indicates that approximately 2–3% of people in North America have scoliosis (studies on scoliosis prevalence). Healthcare providers use a combination of physical examinations and radiographic imaging, particularly X-rays, to assess both the presence and the severity of the condition. The goal is early detection, with regular monitoring aimed at preventing progression that could lead to complications later on.
This condition can affect various parts of the spine depending on the type of curve. In patient groups studied, nearly half of the cases featured double curves, with other common types including thoracolumbar-lumbar and thoracic curves. Understanding the specific type of curvature is critical when determining subsequent treatment methods.
X-Ray Classification: A New Language for Scoliosis
Recent advancements in radiographic analysis have led to a new classification system for scoliosis, particularly in adults. Spine surgeons have long faced challenges when trying to communicate the complexities of the spine’s curvature. A recent system, unveiled in a December 2025 study in the European Spine Journal, helps clarify these complexities by providing a common language that both clinicians and researchers can understand. This approach is particularly beneficial in adult idiopathic scoliosis, where variability in curve patterns demands precise description and categorization (European Spine Journal study on classification).
Dr. James D. Lin from The Mount Sinai Hospital explained that the new X-ray classification system “provides a new language for clinicians and researchers, helping us reliably categorize and communicate the radiographic features of adult idiopathic scoliosis” (Mount Sinai press release). By standardizing terminology, the system significantly improves communication among the various specialties involved in managing scoliosis.
What makes this innovation particularly significant is its ability to capture subtle differences in curve morphology. The precise description not only aids in consistent tracking of curve progression but also assists in customizing treatment plans according to each patient’s unique anatomy. With clearer radiographic features, clinicians can now predict the likelihood of curve progression and decide if a more intensive intervention is necessary.
Unsure what your scan results really mean?
We analyze MRI, CT, PET, Ultrasound, and X-ray reports and deliver a clear, easy-to-understand summary in under 1 minute.
- Understand your results in simple language
- Easy to understand explanations
- Get a list of questions to ask your doctor
Assessing Scoliosis Severity: Beyond the Numbers
X-rays play a crucial role in evaluating the severity of scoliosis. One of the breakthrough findings reported in a December 2025 study focused on the scoliosis severity index found that the index correctly classified 82% of adolescent idiopathic scoliosis patients as either stable or progressive (European Spine Journal severity index study). This tool is more than a mere number; it provides valuable guidance on when to intervene, especially for adolescents whose curves might progress unexpectedly.
The assessment of scoliosis severity using X-ray imaging typically combines the Cobb method with newer classification systems. While the traditional Cobb angle quantifies the degree of curvature, the updated classification systems also provide insights into curve migration and rotation, factors essential for determining the full impact of the deformity on a patient’s health.
Another study involving 94 patients with adolescent idiopathic scoliosis revealed that curve types significantly influence the treatment approach. Approximately 49.8% of patients exhibited double curves, while thoracolumbar-lumbar curves were noted in 25.8% of cases, followed by 16.2% with thoracic curves, and 8.1% with other types of curvature. This information is critical because the type of curve often dictates both the urgency and the nature of the recommended treatments.
Treatment Options: Bracing and Beyond
Treatment of scoliosis varies greatly depending on the severity and type of spinal curvature. In many cases, especially among adolescents, non-surgical treatments such as bracing have proven effective in curbing the progression of the condition. One notable example is the Providence brace, a nighttime spinal orthosis designed to apply corrective pressure through lateral and rotational forces on the spine (Providence brace information on Wikipedia). It plays a key role in preventing further curvature without interrupting normal daytime activities.
Bracing is particularly effective when a patient is still growing. It works best when the physician can closely monitor the curve’s progression through periodic X-ray examinations. The design of the Providence brace, which applies pressure during the night, ensures that mobility is not compromised during the day. This orthosis is a viable alternative for many young patients who might otherwise need more invasive surgical options.
When it comes to adolescents whose curves are classified as moderate or borderline progressive, early detection through X-ray assessment is critical. The precise classification and severity evaluation provided by the latest research allow healthcare professionals to recommend a course of action tailored to individual cases. Whether through bracing, physical therapy, or, in some instances, surgery, treatment strategies are becoming increasingly customized to a patient’s unique curve characteristics.
Navigating Your X-Ray Results
Understanding the details of an X-ray report can be overwhelming, especially when jargon and technical descriptors fill the document. Patients and families are encouraged to sit down with their healthcare provider and ask clear, specific questions about the report’s findings. A well-explained X-ray report enables patients to engage actively in their treatment, whether monitoring a mild curvature or embarking on more significant treatments such as bracing or surgery.
Clinicians now have a more comprehensive toolkit thanks to advancements in radiographic classification. The improved X-ray interpretation not only fosters better communication but also streamlines decision-making about treatment options. A doctor might, for example, use both the scoliosis severity index and the new classification system to articulate how aggressive the treatment plan should be. This dual evaluation approach enriches the conversation between the patient and the healthcare provider and helps set realistic treatment expectations.
Patients are advised to come prepared to ask about how specific curve types might affect their daily activities, potential progression over time, and what conservative measures, such as specific exercises, might benefit their condition. With updated classification systems and evaluation tools, the trend is moving toward more personalized treatment plans that not only incorporate clinical evidence but also account for lifestyle considerations and overall health. This evolution in patient care underscores the importance of understanding one’s X-ray results in detail.
Expert Opinions and the Future of Scoliosis Management
The landscape of scoliosis management is rapidly evolving, driven by innovations in radiographic imaging and classification. Experts like Dr. James D. Lin have been at the forefront of this evolution, emphasizing the importance of a unified classification language for both clinicians and researchers (Mount Sinai Hospital statement). With such advancements, future treatment protocols look promising as they increasingly focus on early detection, prevention, and minimally invasive management techniques.
This future involves not just improved X-ray interpretative frameworks but also a more integrated approach to treatment. The severity index is a prime example of how quantitative tools are used to guide clinical decisions. When these tools are combined with a detailed, up-to-date classification system, they can provide near-real-time answers about whether a patient is likely to experience curve progression. This, in turn, supports more decisive interventions that help mitigate the risk of complications before they become severe.
What is promising about current innovations is the emphasis on personalized care. As additional research is conducted and more data is collected, innovations are expected to lead to even more refined treatment choices that take into account the patient’s unique spinal characteristics. This personalized approach is crucial not just for the adolescent population but also for adult patients who may display distinct radiographic features compared to younger cohorts.
Looking Ahead: Empowerment Through Knowledge
Armed with a comprehensive understanding of their X-ray results, patients are better positioned to engage in active dialogue with their healthcare providers. The evolving narrative around scoliosis management focuses on a collaborative approach, one where patients and clinicians work hand in hand to decide on the best treatment plan.
Empowerment in the context of scoliosis treatment means gaining clarity on the nature of the condition and understanding the significance of each radiographic finding. Clear communication about severity and potential treatment paths enhances patient confidence and leads to better long-term outcomes. With each new study and technological breakthrough, both the diagnostic and communication processes continue to improve.
This modern approach reflects a broader trend in medicine toward personalization and transparency. Patients who have been involved in the process from diagnosis to treatment planning often report higher satisfaction with their care. The ability to understand and interpret one’s own X-ray report is, therefore, not only a technical triumph but also a cornerstone of patient empowerment in a field that historically has been shrouded in technical complexity.
Conclusion: Practical Steps Toward Better Spinal Health
Effectively managing scoliosis involves a clear understanding of both the diagnostic findings and available treatment methods. The blend of traditional methods with modern classification systems significantly improves decision-making in the management of spinal deformities. Advances in X-ray interpretation enable clinicians to provide more precise analysis, ultimately shaping more effective treatment regimens.
For patients navigating a scoliosis diagnosis, taking the time to understand the details of the radiographic report is a critical step. Engaging with healthcare providers about specific terminology and evaluation tools, such as the severity index, clarifies whether conservative measures like bracing are sufficient or if more intensive interventions are needed. The approach underscores personalized care tailored to individual conditions, ensuring that each patient receives treatment that aligns with the nuances of their spinal curvature.
Through the integration of cutting-edge research and improved communication protocols, the journey toward better spinal health is becoming increasingly accessible. Whether examining the new X-ray classification systems or discussing innovative approaches such as the Providence brace, the key is to remain informed and proactive. As research continues to shape the landscape of scoliosis treatment, patients and clinicians alike can look forward to an era where clarity meets care, laying a firm foundation for improved outcomes and a better quality of life.
Waiting for answers? You don’t have to.
Upload your MRI, CT, PET, Ultrasound, or X-ray report and receive a clear explanation in < 1 minute.
Take Control of Your Scoliosis Diagnosis with Read My MRI
Understanding the complexities of scoliosis and its treatment options is crucial for your spinal health journey. At Read My MRI, we're committed to simplifying this process for you. Our AI-powered platform is designed to interpret your medical imaging reports, including X-rays, and provide you with a clear, jargon-free summary. Whether you're deciphering the severity of your scoliosis or exploring treatment alternatives, Read My MRI is here to help you make informed decisions with ease. Get Your AI MRI Report Now! and take the first step towards a clearer understanding of your condition.