TI-RADS 4 or 5 Diagnosis: Is Surgery the Next Step?
A radiology report lands in the patient portal, and one phrase jumps off the page: “TI-RADS 4” or “TI-RADS 5.” For many people, that line instantly sounds like “This is cancer” and “Surgery is next.” The reality is more nuanced. The American College of Radiology (ACR) TI-RADS system was designed to sort thyroid nodules into levels of suspicion and suggest when to biopsy or monitor, not to automatically send everyone to the operating room. An industry report describing how the ACR TI-RADS system stratifies thyroid nodules into categories that guide management decisions makes clear that the higher categories signal concern, but do not stand alone as treatment decisions.
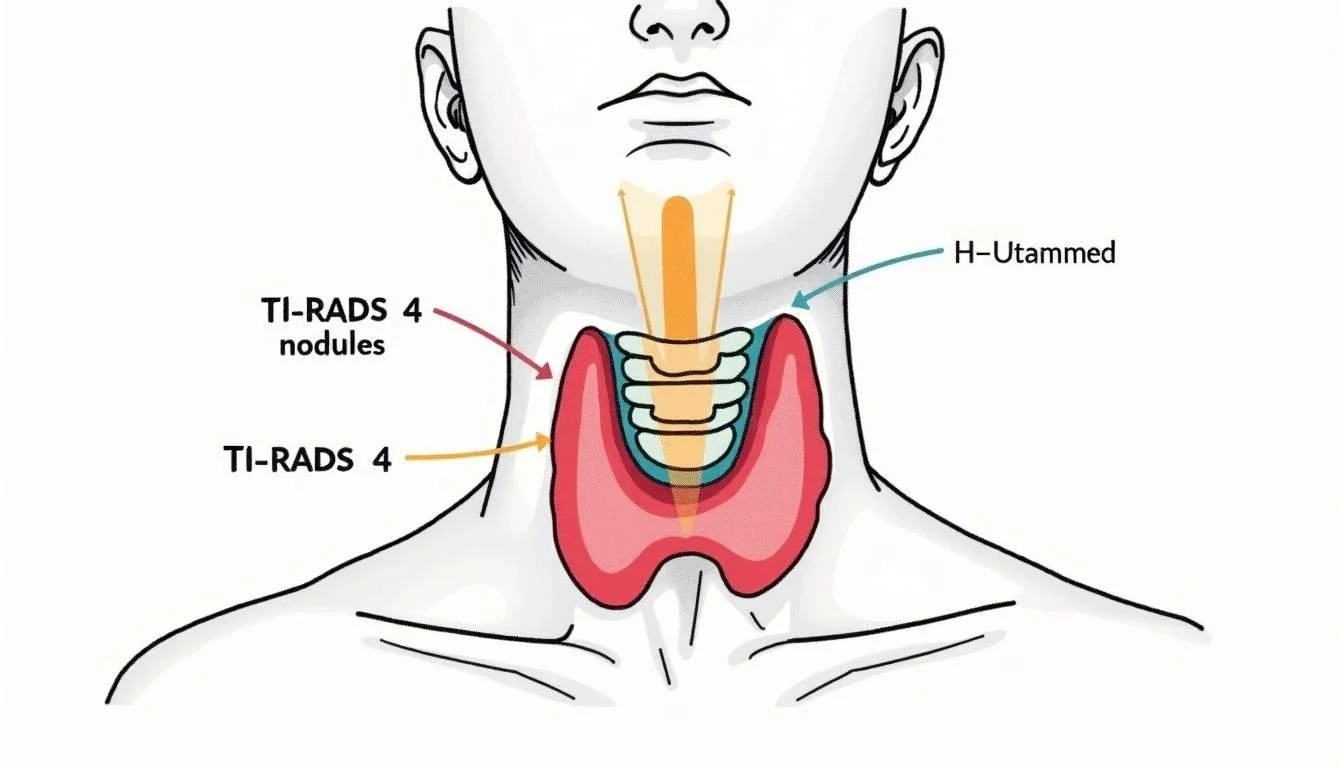
What a TI-RADS 4 or 5 Result Is Actually Saying
TI-RADS is a scoring system radiologists use when looking at thyroid nodules on ultrasound. Features such as how solid the nodule is, how dark or bright it appears, its shape, its margins, and whether there are tiny calcifications all get assigned points. More suspicious features add more points, and the total score gets grouped into a category. TI-RADS 4 is typically labeled “moderately suspicious,” and TI-RADS 5 is “highly suspicious,” meaning the ultrasound appearance raises concern that the nodule could be cancer, but does not prove it.
This distinction matters. The ACR itself stresses that these categories are not a definitive cancer diagnosis. Guidance summarized in the SEER Inquiry System notes that TI-RADS 4 (“moderately suspicious”) and TI-RADS 5 (“highly suspicious”) still require additional evaluation and pathologic confirmation before any cancer determination is made. A TI-RADS 4 or 5 result is a strong signal to look closer with a fine-needle aspiration (FNA) biopsy and clinical review, not a final verdict.
Understanding the implications of a TI-RADS score is crucial for patients and healthcare providers alike. For patients, receiving a TI-RADS 4 or 5 score can understandably lead to anxiety and concern about the possibility of thyroid cancer. It's important to remember that while these scores indicate a higher likelihood of malignancy, they are part of a broader diagnostic process. The next steps typically involve further imaging studies or biopsies that can provide more definitive information. Patients are encouraged to engage in open discussions with their healthcare providers about what these results mean for their individual situations, including potential risks and benefits of further testing.
Moreover, the management of thyroid nodules is a dynamic field, with ongoing research aimed at refining the TI-RADS system and improving patient outcomes. Newer imaging techniques and molecular testing are being explored to enhance the accuracy of diagnoses and reduce unnecessary surgeries. As our understanding of thyroid nodules evolves, the integration of these advancements into clinical practice may help to alleviate some of the uncertainty associated with TI-RADS 4 and 5 results, ultimately leading to more personalized and effective patient care.
How High Is the Cancer Risk with TI-RADS 4 or 5?
Ultrasound categories exist for one reason: to sort nodules into higher and lower cancer risk groups. That risk clearly climbs as the TI-RADS score rises. In one study, researchers reported that nodules in the moderately suspicious category had an estimated malignancy risk about five times that of nodules in a lower-suspicion category, while nodules in the highest category carried a risk about ten times higher than that lower category baseline according to an analysis of malignancy risk across TI-RADS categories. For patients, the takeaway is not that cancer is guaranteed, but that a TI-RADS 4 or 5 nodule sits in a substantially higher-risk group than one labeled TI-RADS 3.
Real-world management patterns reflect that elevated concern. In a study evaluating thyroid nodules, investigators found that, among the nodules reviewed, a large majority of those classified as TI-RADS 4 or 5 went on to surgery, and among the nodules with definitive pathology in that report, malignant cases clearly outnumbered benign ones. That pattern shows how often clinicians decide that higher-suspicion nodules warrant aggressive treatment. Yet even in this kind of study, some nodules were benign, underscoring that TI-RADS can indicate high suspicion without perfectly predicting outcomes for every individual nodule.
Moreover, the implications of a TI-RADS 4 or 5 classification extend beyond immediate surgical decisions. Patients often experience heightened anxiety and stress upon receiving a diagnosis of a suspicious nodule. This emotional burden can significantly affect their quality of life as they navigate the uncertainties of potential cancer treatment. Additionally, the decision-making process may involve multidisciplinary teams, including endocrinologists, radiologists, and surgeons, who collaborate to determine the best course of action based on the patient's overall health, family history, and personal preferences.
Furthermore, ongoing research continues to refine the TI-RADS system, aiming to improve its predictive accuracy. Emerging studies are exploring the integration of molecular testing and advanced imaging techniques to provide a more comprehensive risk assessment for thyroid nodules. These advancements may help clinicians better differentiate between benign and malignant nodules, ultimately leading to more personalized treatment strategies. As the field evolves, it is crucial for patients to stay informed and engage in discussions with their healthcare providers about the implications of their TI-RADS classification and the potential next steps in their care journey.
Is Surgery Really the Next Step After a TI-RADS 4 or 5 Report?
For many people, the fear is that “suspicious” automatically equals “surgery.” In practice, the usual next step after a TI-RADS 4 or 5 finding is a fine-needle aspiration biopsy, not an operation. FNA uses a very thin needle, often under ultrasound guidance, to collect cells from the nodule. Those cells are then analyzed by a pathologist to look for cancer. The result often falls into clear “benign” or “malignant” categories, but sometimes lands in a gray zone, where additional testing or repeat biopsy is needed. This biopsy result, combined with the ultrasound features, blood tests, exam findings, and personal risk factors, shapes whether surgery is recommended.
Guidelines also emphasize that nodule size matters. The ACR recommendations summarized in Current Surgery Reports explain that fine-needle aspiration is typically advised for TI-RADS 4 and TI-RADS 5 nodules once they reach specific size thresholds, while smaller nodules in these categories are often followed with repeat ultrasound rather than immediate biopsy. That means a tiny TI-RADS 4 or 5 nodule in someone with no other risk factors may be closely watched instead of sent straight to biopsy or surgery, especially if it is not causing symptoms.
Even when cancer is confirmed, surgery is still a tailored decision. Some thyroid cancers are small, slow-growing, and unlikely to spread quickly. Others are larger, symptomatic, or show worrisome features such as spread to lymph nodes. Age, other medical conditions, vocal cord concerns, and personal priorities all factor in. A patient who sings professionally might weigh the small risk of voice changes after thyroid surgery differently than someone with a desk job. For many low-risk cancers, partial thyroid removal or, in select cases, active surveillance may be an option, while more aggressive disease may call for more extensive surgery. The key point: the TI-RADS number alone does not dictate the operating room schedule.
Moreover, the psychological impact of a TI-RADS 4 or 5 diagnosis should not be underestimated. Patients often experience anxiety and uncertainty, which can be exacerbated by the fear of surgery. Education plays a crucial role in alleviating these concerns. Understanding that not all suspicious nodules lead to immediate surgical intervention can help patients feel more in control of their health journey. Support groups and counseling services can also provide valuable emotional support, allowing patients to share their experiences and learn from others who have navigated similar paths.
Additionally, advancements in imaging technology and biopsy techniques have significantly improved the ability to assess thyroid nodules. Newer methods, such as molecular testing of FNA samples, can provide further insights into the likelihood of malignancy, helping to refine treatment decisions. This means that even if a nodule is classified as TI-RADS 4 or 5, there may be additional layers of analysis that can influence the management plan. As research continues to evolve, the approach to thyroid nodules will likely become even more personalized, allowing for better outcomes and reduced anxiety for patients facing these challenging diagnoses.
Beyond TI-RADS: Tools That Help Refine the Decision About Surgery
Radiology is evolving quickly, and newer ultrasound techniques are helping to sharpen risk estimates. One recent meta-analysis reported that combining TI-RADS scoring with superb micro-vascular imaging (SMI) - a technique that better visualizes tiny blood vessels - significantly improved the ability to distinguish benign from malignant thyroid nodules by enhancing diagnostic accuracy when TI-RADS was paired with SMI. Better distinction means fewer unnecessary surgeries for benign nodules and more confidence in operating when the signs truly point to cancer.
For someone sitting with a new TI-RADS 4 or 5 result, these advances translate into practical questions to raise with a clinician. It can be helpful to ask: How concerning does this specific nodule look on ultrasound, and why? Is an FNA biopsy recommended now, or is close ultrasound follow-up reasonable? If FNA is done, how will the results change the plan - what would lead toward surgery, and what might mean continued monitoring? Are additional imaging techniques or specialized thyroid ultrasound experiences available locally? Anchoring the conversation in concrete next steps, and in what the care team will do with each possible result, often reduces anxiety and makes the path forward clearer.
Understand Your Thyroid Imaging with Ease
At Read My MRI, we understand the complexity and anxiety that comes with receiving a TI-RADS 4 or 5 diagnosis. That's why we offer a user-friendly platform to help you make sense of your medical imaging reports. Our AI-powered service simplifies your MRI, CT, or Ultrasound reports, providing you with clear, jargon-free summaries. Whether you're considering the next steps after a thyroid nodule evaluation or any other medical imaging concerns, Read My MRI is here to help you understand your options with confidence. Get Your AI MRI Report Now! and take the first step towards clear and comprehensible medical insights.