Dawson’s Fingers on MRI: Identifying MS or Other Conditions?
The phrase “Dawson’s fingers” can stop someone in their tracks when reading an MRI report. It sounds dramatic, and for many people it immediately raises one question: does this mean multiple sclerosis? Dawson’s fingers are strongly associated with MS, but they are only one piece of a larger diagnostic puzzle. A recent consensus report on MRI features in multiple sclerosis describes these finger-like lesions as a classic sign of the disease, yet neurologists always look at far more than a single line on a scan. Understanding what these lesions are, why they matter, and when they can show up in other conditions helps turn a frightening mystery into something more manageable and grounded in evidence.
What exactly are Dawson’s fingers on MRI?
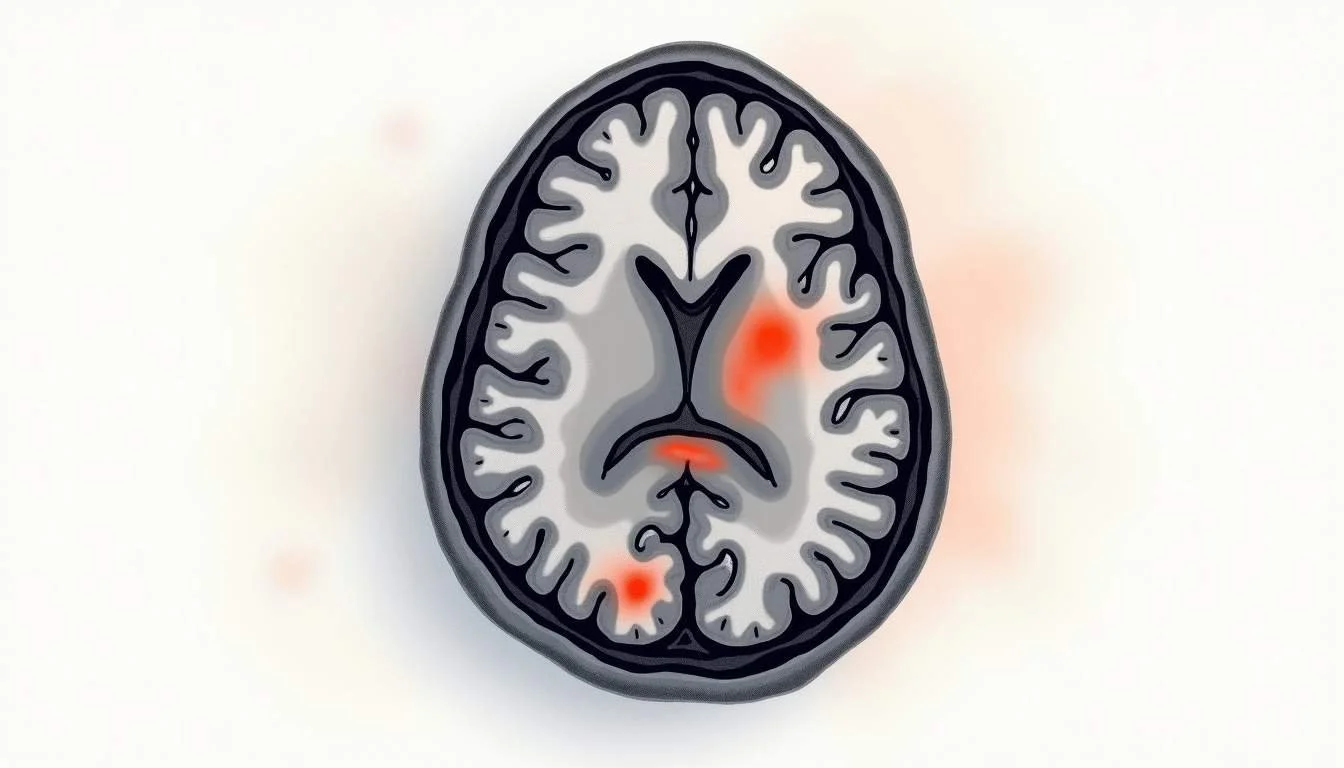
Dawson’s fingers are areas on brain MRI that look like pale, finger-like streaks radiating outward from the fluid-filled spaces in the middle of the brain, called the lateral ventricles. On T2-weighted or FLAIR images, they appear as bright, ovoid lesions that line up along the small veins that run perpendicular to the ventricles. Radiologists call this “periventricular” because the lesions cluster around the ventricles and seem to reach outward into the surrounding white matter like narrow spokes or fingers.
The name comes from Dr James Walker Dawson, a Scottish pathologist who carefully studied the brains of people with what is now known as multiple sclerosis. In his descriptions, he wrote about “wedge-shaped areas with broad base to the ventricle, and extensions into adjoining tissue in the form of finger-like processes,” a phrase still quoted today in explanations of these lesions described by Dr James Walker Dawson. Modern MRI technology now allows clinicians to see in living patients what Dawson originally described under the microscope: bands of damage tracking along veins where the immune system has attacked the insulating myelin coating of nerve fibers.
Why Dawson’s fingers are such a strong clue for multiple sclerosis
Dawson’s fingers matter because they reflect a pattern of damage that fits closely with how MS behaves in the brain. MS is a demyelinating condition, meaning the immune system mistakenly targets myelin, the protective covering of nerve fibers. In MS, that attack often centers around small veins near the ventricles. When inflammation flares in those areas, it can leave behind scars or plaques that align along the veins, creating the elongated shapes seen as Dawson’s fingers. This venous, periventricular distribution is much more typical of MS than of many other neurological conditions that also produce white matter spots on MRI.
Research backs up how common Dawson’s fingers are in people who truly have MS. In one MRI study of people with confirmed multiple sclerosis, Dawson’s fingers were identified in 92.5% of patients by one reader and 77.5% by another, highlighting both their high frequency and the reality that different radiologists may rate the same scans slightly differently MRI study of Dawson’s fingers in MS. When a pattern shows up this often in a well-defined group of patients, it quickly becomes one of the classic clues clinicians look for.
Specificity also matters. Clinicians are not just asking, “How often do we see Dawson’s fingers in MS?” but also, “How often do we see them in people who do not have MS?” A recent case report emphasized that Dawson’s finger hyperintensities are highly specific for multiple sclerosis compared with other demyelinating conditions when seen on a primary diagnostic MRI case report highlighting the specificity of Dawson’s finger lesions. That does not mean the finding proves MS on its own, but it does mean that, in the right clinical context, these lesions carry significant weight when neurologists are deciding whether someone meets diagnostic criteria for the disease.
When Dawson’s fingers don’t necessarily mean MS
Even with their strong association with multiple sclerosis, Dawson’s fingers are not absolutely unique to it. One of the key lessons in interpreting brain MRI is that pattern matters, but context matters just as much. Age, vascular risk factors, prior strokes, autoimmune conditions, infections, and even migraine history can all influence how white matter looks on imaging. Sometimes that background can create lesions that partially mimic the Dawson’s finger appearance, even without MS being present.
Research has shown that Dawson’s finger–like lesions can appear in other conditions that affect small blood vessels in the brain. In one study of older adults with cerebral small vessel disease, lesions resembling Dawson’s fingers were found in 10.5% of participants, suggesting that these finger-like patterns are not exclusively seen in MS study of Dawson’s fingers in cerebral small vessel disease. For patients and clinicians, this underscores a critical point: the presence of Dawson’s fingers is a strong clue but not a standalone diagnosis. Neurologists must weigh how the MRI findings fit with symptoms, neurological examination, spinal fluid analysis, and how the condition evolves over time.
Unsure what your scan results really mean?
We analyze MRI, CT, PET, Ultrasound, and X-ray reports and deliver a clear, easy-to-understand summary in under 1 minute.
- Understand your results in simple language
- Easy to understand explanations
- Get a list of questions to ask your doctor
How doctors interpret Dawson’s fingers in real life
When a radiology report mentions Dawson’s fingers, the next step is not automatically to label the scan as “MS” but to integrate that detail into a broader picture. Radiologists will note not just the presence of these lesions, but also where else lesions appear: in the spinal cord, the cerebellum, the brainstem, or the optic nerves. They consider whether lesions are of similar age or whether some appear more recent than others, suggesting new activity. Neurologists then read the report alongside a careful clinical history. Have there been episodes of blurred vision, weakness, numbness, or problems with coordination that came and went? Are there other medical issues such as long-standing high blood pressure or diabetes that might point more toward small vessel disease than MS?
Modern diagnostic frameworks for MS emphasize “dissemination in space and time”-essentially, evidence that lesions are occurring in multiple characteristic locations and at more than one point in time. Dawson’s fingers contribute primarily to the “space” part of that story, especially for periventricular involvement, but they cannot answer the “time” question on their own. To address that, neurologists might compare a current MRI with older scans, look for lesions that enhance with contrast (a marker of more recent inflammation), or follow a patient with repeat imaging if the initial picture is not yet clear. This stepwise approach helps prevent both overdiagnosis and underdiagnosis, particularly in people whose scans show some features suggestive of MS but whose symptoms or additional tests do not fully fit.
There is also a human side to this interpretation. For someone reading “Dawson’s fingers present” in a report, anxiety is understandable. Experienced clinicians often spend time explaining that MRI findings are pieces of a puzzle, not verdicts. It is entirely possible to have lesions that look worrisome yet never go on to develop MS, just as it is possible to have relatively mild imaging changes but clear clinical relapses. The art of neurology lies in matching the scan to the person sitting in front of the doctor, not to a textbook ideal.
What this means for your MRI report and next steps
Seeing Dawson’s fingers mentioned in an MRI report should be treated as a prompt for a careful, structured conversation rather than as a definitive label. The first step is usually a detailed appointment with a neurologist who is experienced in demyelinating diseases. During that visit, the doctor will typically review not just the written report but also the actual images, often scrolling through them with the patient and pointing out where the lesions are and what patterns they form. Questions about past neurological symptoms, even those that may have seemed minor or were previously attributed to stress or fatigue, become important. So do family history, prior infections, autoimmune conditions, and cardiovascular risk factors.
Depending on the overall picture, the neurologist may suggest additional testing. That can include spinal fluid analysis looking for markers of immune activity, blood work to rule out conditions that mimic MS, or repeat MRI after some time has passed to see whether any new lesions have appeared. For some patients, the answer is relatively clear: the combination of Dawson’s fingers, lesions in other characteristic locations, and a history of episodes fits well with MS. For others, the situation falls into a gray zone often described as “radiologically isolated syndrome” or as non-specific white matter changes that warrant watchful waiting rather than immediate treatment.
For people trying to make sense of all this, a few practical strategies help. Bringing a written list of questions to the neurology appointment keeps the discussion focused: What exactly did the radiologist see? How strongly does this pattern suggest MS versus other explanations in this particular case? What other tests, if any, are needed? And what signs or symptoms should prompt an urgent call if they occur in the future? Clear, specific questions turn an intimidating report into a set of next steps that the healthcare team and patient can navigate together.
Looking ahead: MRI advances, earlier clues, and questions to ask
MRI technology is evolving quickly, and Dawson’s fingers are now part of a wider toolkit for understanding MS and related conditions. Researchers have identified subtle MRI signatures that can appear even before classic lesions like Dawson’s fingers become visible, including changes that reflect early shifts in immune activity and inflammation in the brain. One landmark study reported that specialized MRI techniques could detect signs of a multiple sclerosis–like immune response before conventional lesions appeared, raising the possibility of identifying high-risk patients sooner and monitoring them more closely landmark study on MRI signatures before visible MS lesions. While these methods are not yet part of everyday clinical practice everywhere, they point toward a future where MRI does more than just confirm damage-it may help predict and prevent it.
For someone living through this now, the core message is more grounded. Dawson’s fingers on MRI are a powerful clue but not the entire story. Good care means combining what the scan shows with what the person feels and experiences, then revisiting that picture as new information emerges. Asking whether the MRI pattern truly matches MS, whether other conditions have been carefully ruled out, and how often follow-up imaging is needed can all help keep care personalized rather than one-size-fits-all.
It is also worth remembering that an MRI report is written for clinicians, not as a final verdict for patients. Terms like “Dawson’s fingers” are technical shorthand, not prophecies. When those words appear, the safest response is not to assume the worst, but to seek a clear, thorough explanation from a qualified neurologist. With thoughtful interpretation, ongoing research, and open communication, these strange-sounding “fingers” become less a source of fear and more a useful signpost guiding diagnosis, monitoring, and treatment decisions over time.
Waiting for answers? You don’t have to.
Upload your MRI, CT, PET, Ultrasound, or X-ray report and receive a clear explanation in < 1 minute.
Empower Your Understanding with Read My MRI
If you're grappling with the complexities of an MRI report and seeking clarity on findings like Dawson's fingers, Read My MRI is here to help. We simplify your medical reports using advanced artificial intelligence, providing you with an easy-to-understand summary that cuts through the medical jargon. Our service is perfect for patients who need a clearer picture of their diagnosis and for healthcare providers who require efficient report analysis. Take control of your health journey and Get Your AI MRI Report Now!