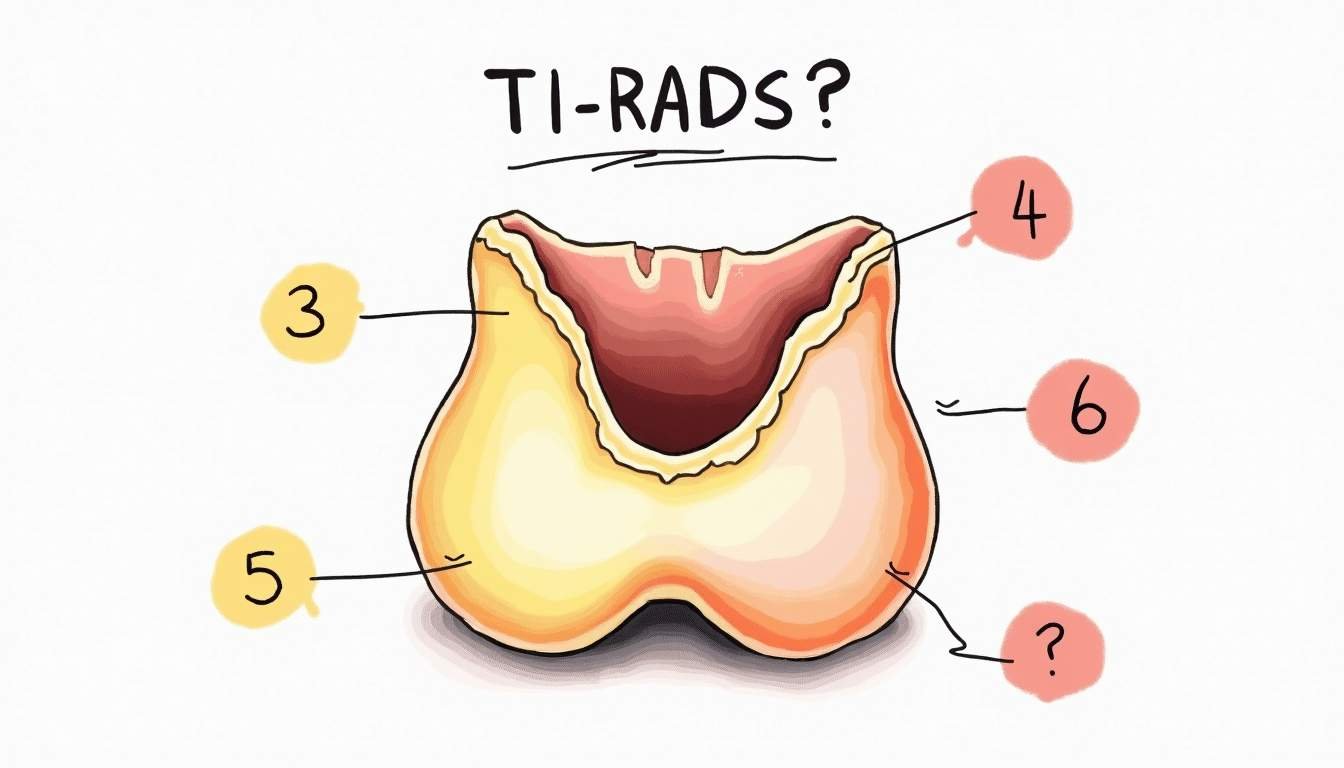
Understanding TI-RADS 3, 4, 5: What Your Score Means and When to Worry
You open your ultrasound report and see: “TI-RADS 3 nodule” or “TI-RADS 5 – highly suspicious.” The words look technical, but the real question behind them is simple: “How worried should I be?” The TI-RADS score is your radiologist’s way of turning the ultrasound picture into a risk estimate for thyroid cancer. It does not predict the future with perfect certainty, but it does give a surprisingly useful range of risk. In a study of 1,000 thyroid nodules, malignancy rates were 0.8% for TI-RADS 2, 1.7% for TI-RADS 3, 16.0% for TI-RADS 4A, 43.2% for TI-RADS 4B, 72.7% for TI-RADS 4C, and 91.3% for TI-RADS 5, showing how sharply the risk rises as the score increases.
What TI-RADS Actually Tells You
TI-RADS stands for “Thyroid Imaging Reporting and Data System.” It is a scoring system radiologists use when looking at thyroid nodules on ultrasound. Instead of writing a free-text description that can be interpreted in many ways, the radiologist assigns points based on features like how solid the nodule is, whether it has bright or dark areas, the shape and margins, and whether there are calcifications. Those points add up to a category, typically labeled TI-RADS 1 through 5.
The system was developed by the American College of Radiology specifically to standardize how thyroid nodules are reported and to guide decisions about follow-up and biopsy, with the goal of reducing unnecessary procedures while still catching cancers early according to the ACR. Instead of every radiologist and every endocrinologist using slightly different thresholds, TI-RADS gives a shared language. When your report says TI-RADS 3, 4, or 5, it reflects a structured assessment, not just a gut feeling.
TI-RADS 3: Mildly Suspicious, Usually Low Risk
TI-RADS 3 is labeled “mildly suspicious.” On ultrasound, these nodules may have some features that are not perfectly reassuring-perhaps they are mostly solid or have subtle irregularities-but they lack the more worrisome patterns that push a nodule into categories 4 or 5. Many nodules in this group turn out to be benign, which is why this category often leads to watchful follow-up rather than an immediate biopsy, especially when the nodule is small and you have no high-risk history.
The malignancy risk with TI-RADS 3 is not zero, but it is relatively low compared with higher categories. In the large series of thyroid nodules where malignancy rates were carefully tracked, TI-RADS 3 nodules had a malignancy rate of 1.7%, far below the risks seen in categories 4 and 5 in that 1,000-nodule study. For many people, that kind of number means the safer approach is periodic ultrasound monitoring to watch for change in size or appearance, rather than jumping straight to a biopsy.
TI-RADS 4: A Wide Range of Risk in One Label
TI-RADS 4 is where anxiety usually spikes, partly because it covers such a broad spectrum of risk. This category is divided into subgroups-4A, 4B, and 4C-based on how many suspicious features are present on ultrasound. A nodule that just barely qualifies as 4A may only have modestly concerning features, while a 4C nodule may look much more worrisome, sometimes only a step below TI-RADS 5 in appearance.
The numbers from structured research reflect that internal spread. In the study that followed malignancy rates across categories, TI-RADS 4A nodules had a malignancy rate of 16.0%, TI-RADS 4B reached 43.2%, and TI-RADS 4C climbed to 72.7%, highlighting why doctors often treat different 4 subcategories differently based on those data. A low-end 4A might lead to careful surveillance or biopsy depending on its size and your personal risk factors, while a 4C nodule is much more likely to prompt a recommendation for biopsy.
Hearing “TI-RADS 4” without the subcategory or context can be confusing. The actual management plan usually considers the sub-score details, the size of the nodule, your age, any history of radiation exposure, and family history of thyroid cancer. Two people with a TI-RADS 4 nodule can reasonably end up with different plans: one monitored with repeat ultrasound, another scheduled for ultrasound-guided fine-needle aspiration biopsy. The category is a starting point for decision-making, not a verdict on its own.
What pushes a nodule into TI-RADS 4
Nodules usually move into TI-RADS 4 when they show several ultrasound features that are each somewhat suggestive of malignancy. These can include being mostly or completely solid, having a darker (hypoechoic) appearance compared with the surrounding thyroid, having irregular or lobulated margins, or demonstrating tiny calcifications. None of these features by themselves necessarily mean cancer, but in combination they raise the level of concern enough to move the nodule out of the low-risk category.
Understanding that process can help the report feel less mysterious. Rather than seeing TI-RADS 4 as a label dropped from nowhere, it becomes the sum of visible characteristics that have been studied and correlated with cancer risk. Your endocrinologist or radiologist can walk through which features your specific nodule has and whether any subtle changes on follow-up scans should change its category over time.
Unsure what your scan results really mean?
We analyze MRI, CT, PET, Ultrasound, and X-ray reports and deliver a clear, easy-to-understand summary in under 1 minute.
- Understand your results in simple language
- Easy to understand explanations
- Get a list of questions to ask your doctor
TI-RADS 5: When Doctors Are Very Concerned
TI-RADS 5 is reserved for nodules that look highly suspicious on ultrasound. These nodules usually have several strong red-flag features together-for example, very dark appearance, a taller-than-wide shape, highly irregular or spiculated margins, and sometimes punctate calcifications. When a nodule scores this high, the probability that it is malignant is substantial, and most guidelines treat biopsy as the default unless there is a compelling reason not to.
In the large cohort where malignancy risk was quantified for each category, TI-RADS 5 nodules had a malignancy rate of 91.3%, the highest of any group and much higher than the TI-RADS 3 and lower 4 categories in that same 1,000-nodule analysis. That does not mean every TI-RADS 5 nodule is cancer, but it explains why doctors typically move quickly to obtain a tissue diagnosis. For people with this score, the main uncertainty is less about whether to investigate and more about planning next steps if the biopsy confirms malignancy.
How Accurate Is TI-RADS – And What About Missed Cancers?
No risk-stratification system is perfect, and patients often worry about both directions of error: nodules that are benign but get biopsied anyway, and nodules that are malignant but scored too low. TI-RADS was designed to lean toward catching cancers, even if that sometimes means more nodules get sampled. In a study involving 195 thyroid nodules, TI-RADS had a sensitivity of 100% for detecting malignancy and a specificity of 61.1%, compared with 100% sensitivity and 75% specificity for the American Thyroid Association risk system in that head-to-head comparison. In practical terms, that study suggested both systems were very good at not missing cancers, but TI-RADS labeled more benign nodules as suspicious.
Other work has looked at ways to refine ultrasound-based risk assessment to improve both sensitivity and specificity. A meta-analysis examining TI-RADS combined with superb micro-vascular imaging reported a pooled sensitivity of 88% and specificity of 89% for distinguishing benign from malignant thyroid nodules, suggesting that carefully chosen add-on techniques can sharpen the signal from ultrasound alone according to that pooled analysis. For patients, this means the headline TI-RADS category is already backed by solid accuracy data, and in more complex cases your team may layer additional imaging techniques to fine-tune the risk estimate.
New Tools That Refine TI-RADS Scores
Radiologists and endocrinologists are not limited to standard grayscale ultrasound when deciding what to do with a TI-RADS 3, 4, or 5 nodule. Newer ultrasound techniques can add information about stiffness and blood flow, which sometimes helps distinguish aggressive cancers from more indolent or benign nodules. These tools do not replace TI-RADS, but they can refine how confidently a given score is interpreted, especially in the gray zones where management decisions are hardest.
One example is three-dimensional shear wave elastography, a technique that measures how stiff the nodule is in three dimensions. A 2023 study found that combining ACR TI-RADS with three-dimensional shear wave elastography improved diagnostic efficiency for nodules already scored as TI-RADS 4 or 5, offering a more precise way to separate benign from malignant in that higher-risk group in that elastography study. Another approach uses superb micro-vascular imaging to analyze very small blood vessels within the nodule; when this was layered with TI-RADS, the previously mentioned meta-analysis showed balanced gains in both sensitivity and specificity for cancer detection based on its pooled results. If your report mentions these techniques, it usually means your team is using every available tool to avoid both missed cancers and unnecessary biopsies.
When to Worry, When to Watch, and What to Ask
Knowing your TI-RADS score helps, but it does not answer every question about what happens next. A TI-RADS 3 result often leads to scheduled follow-up scans to watch for change, while higher TI-RADS 4 and 5 scores more frequently prompt biopsy recommendations. At the same time, your personal situation matters: age, other medical conditions, family history, and your own tolerance for uncertainty all shape the plan. In real-world practice, the ACR’s TI-RADS guidelines have been reported to “dramatically” reduce unnecessary thyroid biopsies by standardizing when to monitor and when to sample nodules according to an industry report on TI-RADS adoption, which is reassuring if your doctor recommends watching a low-risk nodule instead of immediately biopsying it.
For your own peace of mind, it helps to walk into appointments with clear questions. Useful ones include: What exactly made my nodule TI-RADS 3, 4, or 5-can you show me the features on the images? How does my score, along with the size and location of the nodule, influence whether you recommend biopsy or surveillance? Are there additional imaging tools, like elastography or advanced blood-flow imaging, that could clarify the risk in my case? Finally, ask how often you should be rechecked and what specific changes would trigger a different plan. TI-RADS is a powerful tool, but it is still just one part of a broader conversation between you and your medical team about risk, reassurance, and the right amount of intervention.
Waiting for answers? You don’t have to.
Upload your MRI, CT, PET, Ultrasound, or X-ray report and receive a clear explanation in < 1 minute.
Take Control of Your Health with Read My MRI
Don't let complex medical terminology add to your concerns. At Read My MRI, we empower you with clear, AI-generated summaries of your MRI, CT, PET, X-Ray, or Ultrasound reports. Our service is designed to demystify your medical data, providing you with the understanding you need to make informed decisions about your health. Whether you're facing a TI-RADS 3, 4, or 5 score, or any other medical report, clarity is just a click away. Get Your AI MRI Report Now! and step into a world where your medical reports are accessible and understandable.